Within Sight:
How global tech developments aim to return sight to the blind
By Peter Rukavina and Robert Williams
Be it a baby’s first steps, a wedding day smile, or a spectacular, setting sunset — life is made of visual moments. For the millions faced with visual impairment, there ways to function in a world without sight, but there are also experiences that cannot be replaced.
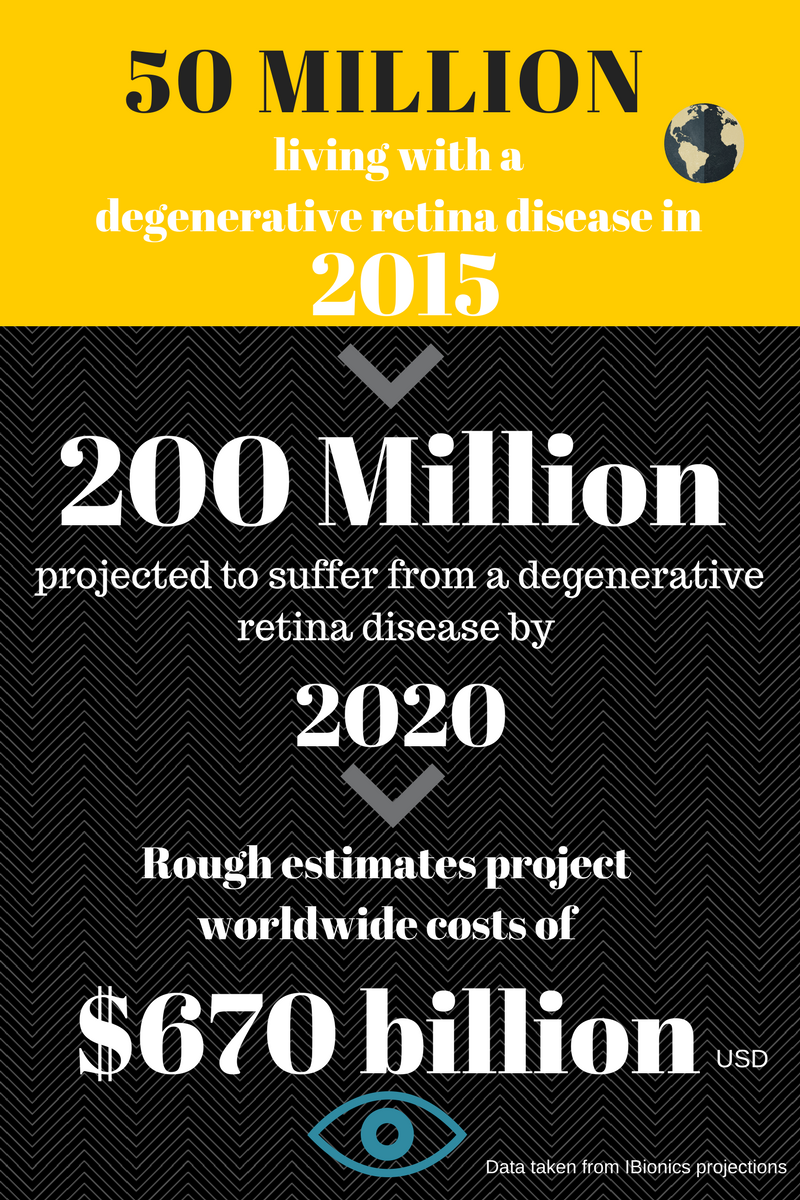
The burden of degenerative retina disease is a growing concern around the world as the number of people disabled is expected to quadruple in the coming years.
Thanks to developing implant technologies, prospects are changing for those that will have their eyesight diminished. There are local and international groups who envision a future where the aid of braille and walking canes are not needed.
Researchers are currently testing retinal implants with hopes of restoring the sight millions have been robbed of. Two companies, Ottawa’s iBionics and the Italian Institute of Technology (IIT) have respectively been working to develop near-microscopic technologies that could be implanted behind a human eye stricken with age-related macular degeneration (AMD) or retinitis pigmentosa (RP).
“It’s the idea of interfacing with the body’s electrical system and hacking into the body to get it to do the things that you want it to do,” says Steven Prawer, co-founder and chief technology officer for iBionics. “We are prepared to do something innovative and something that will change the world.”
Through a wireless, diamond-encased retina chip, iBionics is making its case for a widely-accessible aid that can be easily and regularly implanted. Meanwhile, the IIT’s organic replacement retina is on its way to sharing its animal-stage success with human test subjects.
With every inch of progress, these unrelated groups of scientists are moving towards a market that is deprived of a higher quality of life and has only seen minimal visual improvements through protruding, invasive eyewear.
“It would most certainly be a game changer and allow for much greater definition,” says Dr. Keith Gordon, vice president of research at the Canadian National Institute for the Blind (CNIB). Gordon explains that when compared to the only currently-approved technology – a pair of camera-mounted glasses called Argus II that allow users to differentiate between dark and light – these two groups could give patients the ability to see distinct qualities of an image.
The Blind Spot
The target market for the two forms of implants includes a variety of people suffering from retinal diseases.
The elderly are primarily affected by AMD, which causes a blurred central vision and distorted direct line of sight . The progressive disease is caused by the death of photoreceptor cells that natural convert light into electrical impulses for the brain.
In contrast, RP can strike at a much younger age. As an inherited retinal disorder, RP commonly affects younger to middle-aged people. With it, they initially experience a decline in their peripheral and night vision, only to eventually see failure in their colour perception and central vision as well.
But with surgical solutions far and few between, those living with developed cases of AMD or RP face physical and financial challenges that force them to a lesser quality of life, and a forced change in habits and practices.
Scientists understand that the current state of these prospective solutions will not lead to a completely refined and clear eyesight, but the aim is that these technologies can give those with disabled vision a chance to be independent.
The Diamond Eye
Having been on the market for nearly 20 years, the assisting option of camera-mounted glasses isn’t particularly new technology. What is new, however, is the way the camera’s image is delivered.
Straying from competitor designs that employ a small, electrical wire that carry a current into the eye socket and attach to a pair of glasses, iBionics has built its product with a distinct difference: wireless technology. This wireless difference, according to Prawer, removes one of the most limiting aspects of the existing technology because of it’s superior electrical capacity and reduced chance of infection. “We wanted to start with the surgeons and their difficulties with existing products on the market. Implanting a wireless chip is far easier,” says Prawer.
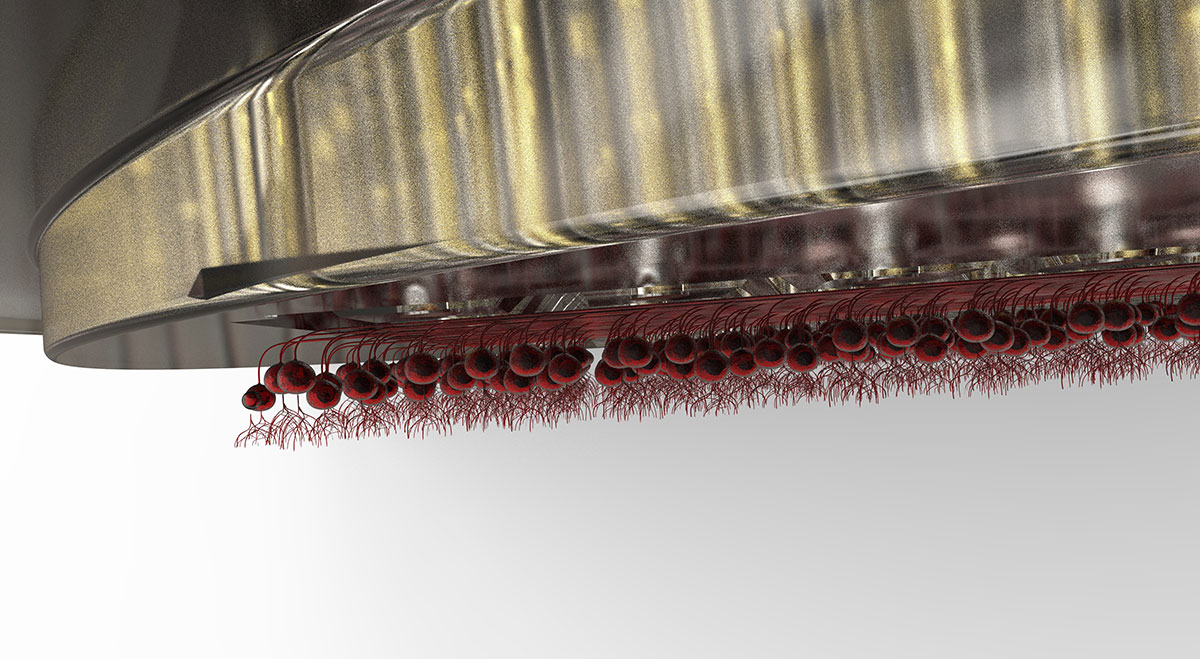
A collaboration between the University of Melbourne, University of Ottawa, and other Canadian academia led to the creation and development of a diamond encased chip that is implanted on the inside surface of the retina. This diamond, which is infused with nitrogen for better electricity regulation, provides a strong, long-term casing and higher electrical stimulation for the microchip.
After receiving a laser signal from the exterior glasses, the diamond chip then converts the light into electricity, stimulates interaction between the retina and the brain, and produces a cloudy, yet dramatically improved image.
With the surgical implantation, the device is estimated to cost $75, 000 CAD. As Prawer explains, the cost factors the betterment of one’s life as well as the removal of other costs instigated by the degenerative diseases.
Replacing the Retina
Contrary to the bionic eye’s mechanized implant, the IIT claims a natural link to restoring vision.
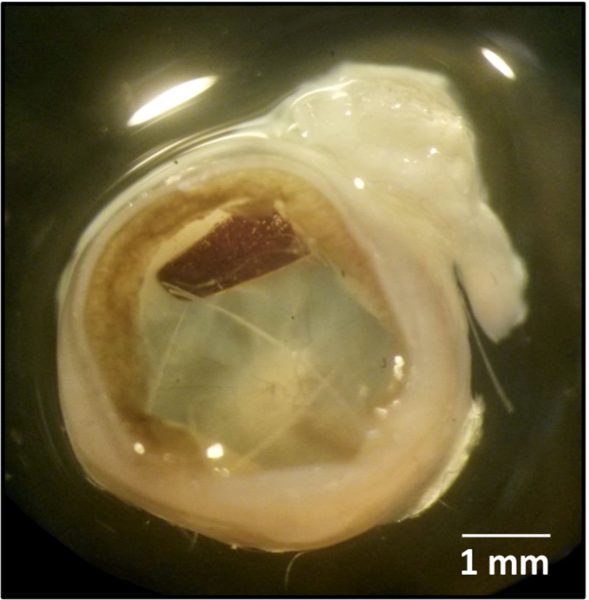
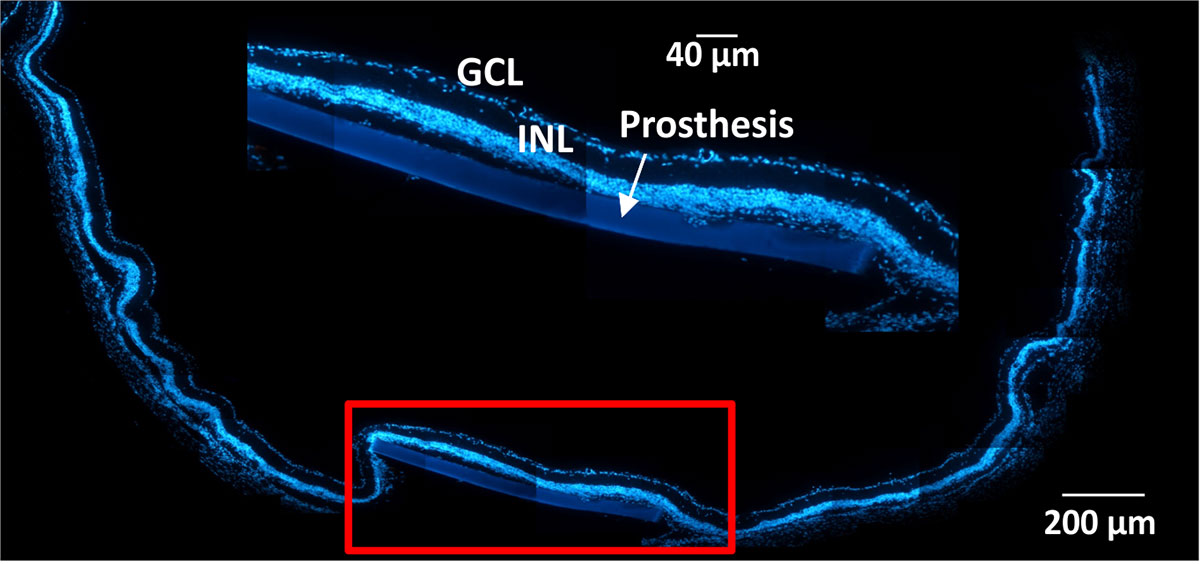
Conductive and semi-conductive polymers, which are made up of organic molecules, are layered around a silk-based substance. Together, they convert light into electricity, stimulate the retina, and complete an image that was partially distorted by disease.
“Our device is extremely simple and it’s organic,” says Fabio Benfenati, a professor of neurophysiology at the University of Genova and an IIT research director. Benfenati notes that polymers, which, in this case, are strings of natural molecules that make up an organic substance, are very friendly to use and they do not ellicit any reaction.
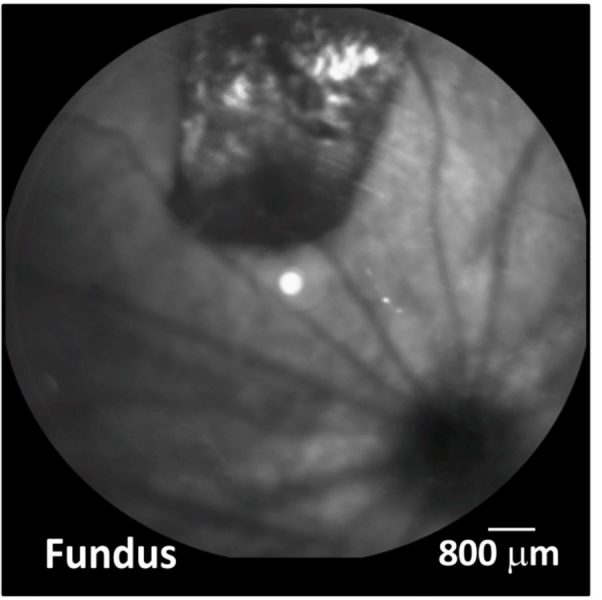
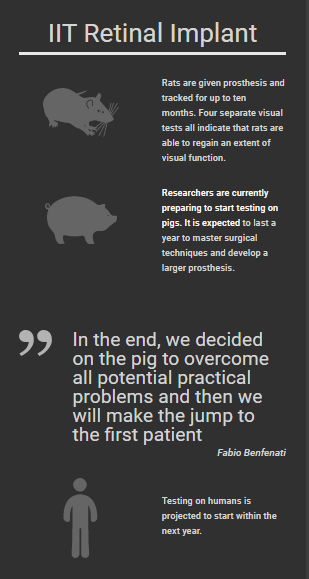
In their recent Nature Materials publication, the IIT identified a group of rats that were implanted with the artificial retina and tested over the course of six to ten months. When compared to healthy rats and their sensitivity to light, the implanted test subjects showed nearly identical results.
“This information is strongly suggesting that the device that we put in place of the dead photoreceptor cells was able to rescue an extent of the visual function,” says Benfenati, whose team will move to pigs for testing before making their way to human experimentation.
Looking ahead
Although both groups have received recognition for the tremendous strides they have made, there is still a long way to go.
Testing, approvals and evaluations can, and likely will, extend the completion of a product for many more years. But as Prawer explains, many of these pursuant scientists are still looking ahead. Not just towards restoring retinas, but towards the countless areas within the human body that struggle to heal through modern therapeutics. All in all, it’s an agenda of smart, electric medicine.
“People are now looking across the whole of the body for where we can stimulate chronically for the benefit of patient health. It’s not just for blindness, but for depression, epilepsy, Parkinson’s disease, improved learning outcomes and so on. This idea of putting smart things in the body is a part of a global reach that will last for a long, long time.”