Doctors must assert independence from drug companies, MPs told
Independence and transparency are crucial to avoid conflict of interest between the pharmaceutical industry and doctors, health experts said Tuesday.
“Doctors are trained and socialized to think that we are special, that we are better human beings than other people,” Thomas Perry, an internal medicine and clinical pharmacology specialist at the UBC Hospital in Vancouver, told the House of Commons health committee. “It’s very difficult for us as a species to come up with the idea that we might be bought or conflicted or influenced.”
Perry, said he got used to declaring conflicts of interest as an elected official in British Columbia, which has strict conflict-of-interest rules. It was only when he returned to UBC, he said, that he realized his former medical colleagues were not used to declaring these conflicts.
Conflict of interest can arise when doctors receive benefits from the drug industry to prescribe a certain medication without knowing whether there is a better product on the market, noted Ramez Ayoub, a Liberal member of the committee.
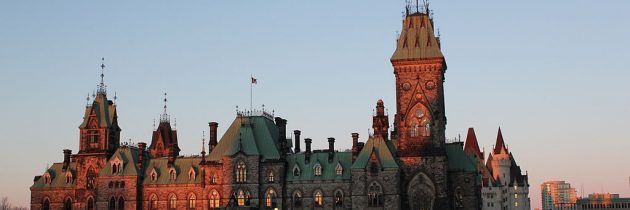
Doug Coyle, a medical professor at University of Ottawa, suggested several steps that could be taken to address conflicts, including independent experts making decisions about drug coverage, and an oversight body to ensure the experts are adhering to principles of fairness and transparency.
Coyle, the interim director of the School of Epidemiology, Public Health and Preventive Medicine, also stressed the importance of finding experts outside of the pharmaceutical industry.
“Don’t believe the argument from the pharmaceutical industry that those who have pharmaceutical money are the experts,”said Coyle.
The issue of conflict of interest arose earlier this year, when Matthew Herder, associate professor at the Faculties of Medicine and Law at Dalhousie University, submitted a brief to the committee emphasizing the need for institutional independence.
“Those charged with making drug coverage decisions must not simply disclose real or potential conflict of interest; instead, they should be conflict free,” wrote Herder.
The committee also heard testimony on the need to properly educate doctors on pharmacare to ensure its success.
“If we are going to go ahead with a national pharmacare strategy, the decision has to be that there is physician education as a key component,” said Coyle.
Perry echoed Coyle’s testimony and said that as drug therapy becomes more complex, physicians’ understanding is falling behind.
“This is something that will require enormous effort to undo,” he said.
Pharmacare is a system of public insurance coverage for prescription drugs. Under the Canada Health Act, “medically necessary services” which includes drugs administered in hospitals are free of charge. However, prescription drugs used outside hospital settings are not free.
A May 2013 survey entitled “Canadian Views on Prescription Drug Coverage” found that 78 per cent of Canadians support the idea of a universal public prescription drug insurance program.
The committee has been tasked with the development of a national pharmacare program.