Improving the patient experience
Every second Wednesday, Zeno Jaworski takes her son Tommy, who suffers from catatonia, to The Ottawa Hospital for his ECT treatment.
They arrive by 6:45 a.m. and immediately head into a special locker room, where Tommy can go to the washroom and change into his hospital gown.

Tommy getting into his hospital gown in the changing room (Photo © Hayley Chazan)
They are then ushered to a special waiting room with comfy chairs. Tommy sits down and listens to his music.
The room is both quiet and comfortable. For Tommy, it’s also familiar. He’s been receiving ECT in the critical care wing of the hospital’s general campus for the past 10 years. And every time he comes in for a treatment, it’s the same song and dance.
“The routine and consistency is very important for Tommy,” said Zeno. “It helps calm his pre-ECT jitters.”
With U.S. soft-rocker Jack Johnson singing softly through his headphones, Tommy sits back, relaxes and closes his eyes.

Tommy listening to music in the waiting room (Photo © Hayley Chazan)
About 45 minutes later, Melinda, the ECT nurse, comes in and escorts Tommy and Zeno into the hospital’s surgical unit, where he waits to be prepped.
The surgical area is massive and modern looking. It contains about 20 gurneys, all lined up in a row, where patients wait to be treated. Only a handful are there for ECT.
The room is quiet in the early morning hours, making it easy for Tommy and Zeno to chat softly.
Sporadically, Melinda will come by and check in. Paul, the assistant to the anesthesiologist, also stops by to say hi; at the same time, he puts in Tommy’s IV.

Tommy in the surgical unit waiting area (Photo © Hayley Chazan)
At The Ottawa Hospital, ECT is delivered three times a week — every Monday, Wednesday and Friday. Both inpatients and outpatients are accommodated. The ECT clinic, as it is known, is only open for a short period of time on these days and the procedures are always performed first thing in the morning, to make room for other, higher priority procedures.
On this morning, Tommy is the second person in line to receive ECT. When it’s his turn, he’s wheeled into a special room, which contains all the equipment needed for the procedure. Also in the room is Dr. Kiran Rabheru, Tommy’s longtime psychiatrist, Paul, Melinda and the anesthesiologist. A medical student accompanies Rabheru and observes the procedure.

Tommy getting wheeled into the ECT procedure room (Photo © Hayley Chazan)
Zeno stays with Tommy until the procedure gets underway, at which point she slips out and closes the curtain that separates the procedure room from the larger surgical unit. At this point, only Tommy, Rabheru, Paul, the anesthesiologist, Melinda and the medical student remain. The anesthesiologist places an oxygen mask over Tommy’s face and within a few moments, he is completely out. Melinda places a bite block in Tommy’s mouth and secures his head and chin, to make sure he doesn’t move or bite is tongue during the seizure. Rabheru then delivers the electrical stimulus.

Tommy inside the procedure room (Photo © Hayley Chazan)
About five minutes later, when the procedure is over, Tommy is wheeled back into the larger unit. The anesthesia wears off quickly; an orderly helps him get dressed and offers him apple juice and some breakfast.
He is then reunited with Zeno, who waits for him patiently in the ICU waiting room. Tommy’s still a little groggy, but he’s well enough to walk on his own. The whole process — from arrival at the hospital until they’re back to the car — takes between two and three hours. Before long, Tommy is back home in bed.
While ECT at The Ottawa Hospital operates smoothly and is well organized, with designated rooms and a sufficient amount of privacy, offering patients a comfortable and relaxing experience, this is unfortunately not always the case at other facilities.
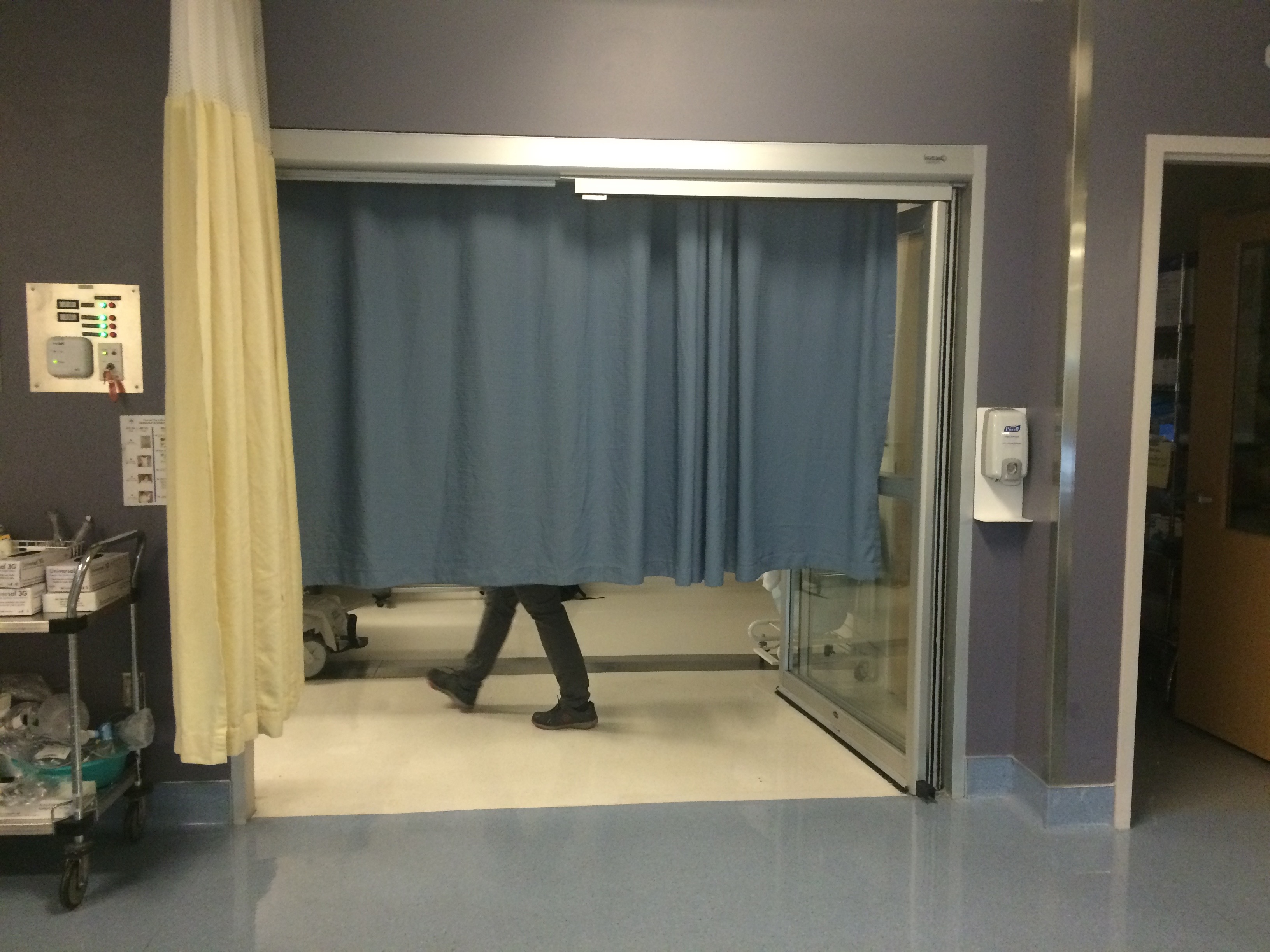
The ECT procedure room is blocked off by a small curtain (Photo © Hayley Chazan)
Dr. Nicholas Delva, head of psychiatry at Dalhousie University in Nova Scotia and chair of the 2006 Canadian ECT survey, said ECT facilities vary significantly, depending on an institution’s location and resources.
“ECT has a high priority in single-specialty psychiatric hospitals and in those locales, there’s not too much of a barrier, and high caseload volumes can be handled,” Delva said. “But in some of the smaller places, ECT might be a lower priority and might have to be done by some arbitrary hour in order to make space for other medical procedures.”
The Royal, a centre in Ottawa devoted exclusively to mental healthcare, fits this description. As a single-specialty psychiatric institution, ECT is delivered three times a week, from 8 a.m. to 12 p.m., but treatments can sometimes go as late as 2 p.m., depending on the demand. Because the clinic doesn’t compete for space with other higher priority surgeries, as is the case at The Ottawa Hospital, psychiatrists can accommodate more patients.

The pre-ECT waiting room at The Royal is closed off from the rest of the hospital and offers patients a lot of privacy (Photo courtesy of The Royal)
The ECT clinic at The Royal has its own designated area, which is tucked away and not visible to the public. At The Ottawa Hospital, the clinic is part and parcel of the larger surgical unit.
While both The Ottawa Hospital and The Royal offer state-of-the-art ECT, the facilities clearly differ.
In rural and remote communities, such as Newfoundland and Labrador, where one has to drive five hours on average just to reach an ECT centre, the facility might be very basic. With fewer resources, there may be less space dedicated to ECT. And with fewer staff, the facility likely can’t accommodate as many patients.
The survey revealed striking differences between ECT centres, in many areas of practice. As a result, Delva and a group of psychiatrists from across the country decided that something needed to be done in order to ensure a more standardized form of ECT, which they believed would improve both the quality of care and the patient experience.
Using the survey findings and best practices from years of experience in the field, Delva and a team of ECT practitioners embarked on a journey to create a standards document that would significantly raise the bar for ECT in Canada. While the guidelines covered multiple areas relevant to ECT, such as training, equipment, treatment technique and follow-up care, Delva was responsible for the guidelines relevant to “facilities and environment.” A draft version of the guidelines has been penned and is currently undergoing peer review. In particular, Delva’s section focused on the space a hospital dedicates to ECT services and how that space should best be allocated to ensure the highest quality of care, both from the point of view of the patient and the treatment team.
Facilities and environment standards
Delva said that what’s most important is that the standards are practical and achievable so that all facilities, big and small, can comply.
“Now we have to keep in mind that some of the sites are going to be low-volume and they’re not going to do as much ECT, so they may not have all the facilities of a big centre,” Delva said. “In these cases, it’s important to remember that ECT in a somewhat cruder environment in some rural type facility is better than no ECT at all, as long as the standards are good.”
Delva’s challenges are many. In establishing the facilities and environment guidelines – and other categories identified for standardizing ECT treatment in Canada – Delva is up against the country’s vast geography, the inevitable limits to healthcare funding and the limited time and energy available among psychiatric doctors to help shape and implement reforms, all while managing their own heavy caseloads.
Furthermore, at general hospitals, where ECT is viewed as a low priority procedure, psychiatrists often face resistance from hospital administration when they try to expand their ECT services. This makes it difficult for practitioners to increase their clinic hours and not all patients in need can be accommodated. It is also a challenge to secure the dedicated space required to perform ECT at a high level.
But despite the obstacles, Delva is hopeful that overtime, the standards document will help practitioners get the resources they need in order to provide the type of care and the volume of care necessary to accommodate all patients in their service. Delva believes that the support of a national organization like CANECTS will help give ECT more credibility in the eyes of hospital administrators.
Delva said that while he’s proud of the group’s work on the guidelines, it is only the first step in what he hopes to be a continuous cycle of improvement in the field of ECT. Once the standards document is reviewed and finalized, the plan is to start undertaking audits of ECT facilities across the country. While the details have yet to be worked out, experienced ECT practitioners, known as accreditors, would visit hospitals in different regions of the country to evaluate the ECT facilities against the guidelines. The centres found to be in compliance with the standards would receive accreditation certifying that they are delivering ECT at the highest possible level.
Delva said that a high-quality peer assessment process is part of the recipe for good performance. He said that while it’s important to have a critical third-party accreditor evaluating each facility, the goal of the audits wouldn’t be to reprimand hospitals, but rather to help them improve.
“Transparency and clarity on what’s happening is very important with ECT, so the public knows what’s happening and it’s all open and above board and done to the highest possible standards — to reassure the public,” said Delva.
